WHAT’S a man to do? Equally important, what’s a doctor to advise when the PSA test is reported elevated? Or should men even be screened for this test? During the last 10 years there’s been considerable flip-lopping about it. Now a large study from the United Kingdom, reported in The Journal of the American Medical Association has new recommendations about PSA testing.
First, this shocking finding. The study showed that men who take the PSA test are just as likely to die of prostate cancer as those who do not have the test! Moreover, some men who do take a PSA are exposed to unnecessary treatment and develop complications that are very annoying.
It’s also worth knowing that if the test is positive for prostate malignancy, it may be wrong. The elevation may be due to an inflammation of the gland, increased size of the prostate (benign prostatic hypertrophy), having sex 24 hours before the test. There’s even some evidence that riding a bicycle 48 hours before the test can increase PSA.
So what’s new about the British study? First, it’s a large one of 400,000 men, aged 50 to 69. Part of the group agreed to a one-time test. Of this group 11 percent had abnormal PSA and most agreed to a biopsy. Another group of the same age range were not offered a test and served as a control group. Ten years later the number of men who had died of prostate cancer was nearly identical.
So what should men do? The decision to have, or not have, the test must always be left to the patient and his doctor. The general consensus among experts is that men should ask their doctor about testing at age 50. But males at higher risk should start earlier. And that, if the decision is to test, it should continue every 2 to 4 years until age 75.
This statistical study questions whether it’s prudent to screen men with the PSA test who do not have any problems. Professor Fuller Albright, one of Harvard’s brilliant minds, would say, “If you have to prove something by statistics, it’s usually wrong.”
Dr. Willett Whitmore, a world authority on prostate cancer, added sage advice many years ago. He said “Getting older is invariably fatal, cancer of the prostate only sometimes. In addition, survival has little to do with treatment”. Whitmore added,” Survival has little to do with treatment. Rather it’s related to the biological nature of the cancer.” In other words, some prostate cancers are pussy cats, others act like raging tigers.
A cardinal principle of medicine is, “First, do no harm.” Good advice, but easier said than done. For instance, autopsies show that prostate cancer in some cases is like graying hair. By age 40 one in three men have evidence of microscopic prostate cancer and 50 percent by age 80. Later in life, these men may die of other diseases.
But if you treat these patients some will develop impotence or urinary incontinence. So both doctor and patient have to be a bit of a philosopher when deciding for or against treatment. The big decision is: Is it better to live with the devil you know than the one you don’t know?
A 70-year-old tennis friend had several normal prostate biopsies and one that showed microscopic cancer. I urged him not to have surgery. But he could not accept having even a scant trace of cancer. He died of a pulmonary embolus while waiting for his wife to drive him home from surgery. He could have lived another 15 years without treatment.
Finally, what’s a man and a doctor to do? It largely depends on the amount of risk patients are willing to take. Some people are convinced the PSA test saves lives. Others are not so sure and believe the PSA test leads to biopsies, potential treatment and complications. But this decision also means they may die of prostate cancer.
So it remains a terrible dilemma, one that can only be decided after a full discussion between the patient and his doctor.
Online docgiff.com
For comments info@docgiff.com
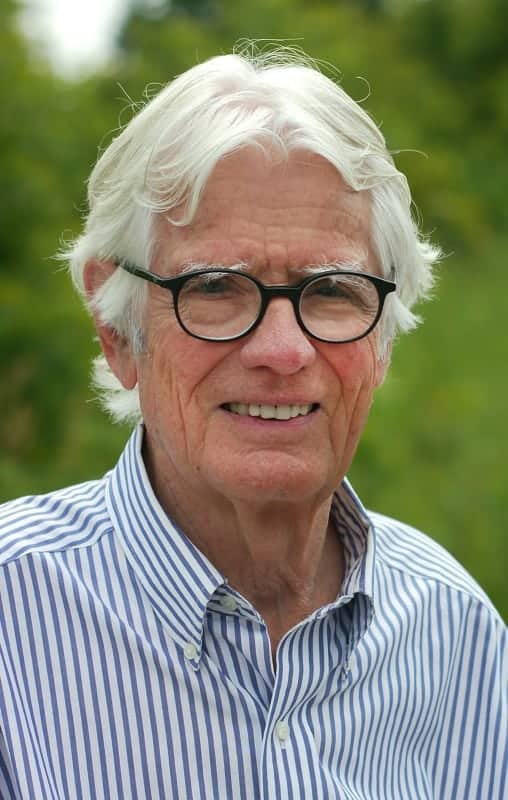
Dr. Ken Walker (Gifford-Jones) is a graduate of the University of Toronto and The Harvard Medical School. He trained in general surgery at the Strong Memorial Hospital, University of Rochester, Montreal General Hospital, McGill University and in Gynecology at Harvard. He has also been a general practitioner, ship’s surgeon and hotel doctor. His weekly medical column is published by 70 Canadian newspapers and 12 in the U.S. The readership is six million. He is the author of nine books.